
Tension-free vaginal tape for stress incontinence in women
Stress incontinence causes involuntary leak of urine during coughing, sneezing, jumping, laughing or during strenuous physical activity. Stress incontinence is caused by prolapsed or mobile urethra and also when the internal urethral sphincter (closure mechanism) is damaged.
Tension-free vaginal tape (TVT) operation provides support for the mobile, prolapsed or sagging urethra so that if your abdominal pressure rise as in coughing, jumping or sneezing or moving suddenly, the urethra is kept closed with no accidental leak of urine.
A small incision is made in the front wall of the vagina. The vagina is separated from the urethra. The mesh-like tape is passed on each side of the urethra close to bladder wall and behind the pubic bones with the help of special needles to two small incisions just above the pubic bones in the lower abdomen. The tape is checked that it is in place and not through the urinary bladder with the help of a cystoscope. No sutures are required to hold the tape in place.
The mesh-like tape supports the urethra like a sling or hammock to keep it in its normal position.
TVT surgery takes approximately 25-40 minutes and may be done under local, spinal or epidural anesthesia.
The surgeon will ask you to cough to allow adjusting the tape to ensure that you are not leaking urine when you cough.
TVT surgery can also be done under general anaesthesia
Tension-free vaginal tape is
Safe
Relatively simple
Relatively non-invasive
Requires minimal hospitalization
Has short recovery time.
Effective as it relieve stress incontinence in 85-90% of cases.
Eighty per cent of obese women or those who have increased pressure on the bladder are cured of stress incontinence after TVT.
TVT can be combined with uterine or vaginal prolapse surgery. Recovery then will be longer.
Tension-free vaginal tape procedure is not done for pregnant women or for women who have a urinary tract infection.
Prior to surgery you can improve the likelihood of regaining continence after surgery by
· Losing weight if you are overweight
· Quitting Smoking if you are smoker. If you would like help to stop smoking before you come into hospital there is a
smoking cessation help line that you can call on. We can also offer Nicotine Replacement Therapy (patches) to patients
who want it.
· Doing Pelvic Floor (Kegel) Exercises. It is usually the first step in managing mild symptoms of SUI. Cure rate can be up to
70%. Or
· Having Magnetic Waves Maximal Perineal Stimulation
Initial Consultation Before having Incontinence Surgery
Full bladder, bowel, gynaecological, medical, surgical, familial, allergy and social history is obtained. General and Specific i.e. gynaecological and neurological examinations are performed. Urine sample is obtained to exclude urine infection. Bladder and urethral prolapse and function are assessed with Cysto-Urethro-Gram and Urodynamics. An ECG and Chest X-Ray maybe ordered.
Before coming to Hospital
Please leave your jewellery at home. If you wish to keep your wedding ring on or you are unable to remove it a protective tape will be placed over it.
Please have a shower or a bath before you come to the hospital.
Eating and Drinking Before Surgery
For morning surgery you will not eat or drink from midnight onwards.
For afternoon surgery you can have a light breakfast of cereal and toast at 6-7 am and nothing to eat or drink until surgery.
What to bring to Hospital
·Medicare card, health fund card, credit or eftpos card and a small amount of money.
·Please bring admission papers if not already sent to hospital.
·Please bring a gown, nightwear, loose day clothes, loose fitting underwear, towels, sanitary towels, personal hygiene items, slippers, magazines and books.
·Please bring with you any tablets or medicines you may be taking.
When to Come to Hospital
You will come into hospital 2 hours before your operation unless instructed otherwise.
You will be shown your bed, change into a gown and have an identity wristband. You will be checked with basic tests such as pulse, temperature, blood pressure and a urine sample.
You would have been told prior to admission if you need to stop taking your medication or if you need to take them on the day of the operation.
You will need to remove glasses or contact lenses and false teeth.
You will be seen by the Anaesthetist. The anaesthetist will ask you about any chest problems, dental treatment and previous anaesthetics you might have had. The anaesthetist will also ask you about any anaesthetic problems within your family. The anaesthetist may order further investigations before or during surgery.
You will be seen also by your Surgeon and his Assistant. The surgery would have been already fully explained to you and you would have also had the consent already signed. If you have any question about the surgery this is your last chance to ask.
After Your Surgery
After the surgery recovery team will take you to the recovery room.
After General Anaesthesia
You will come round i.e. be conscious, a minute or two after the operation ends. Once breathing on your own and awake and you will be transferred back to your room. You are, however unlikely to remember anything until you are back in your bed in your room.
After Surgery You may have a:
· Drip: narrow tube into a vein to give or replace lost fluids
· Facial mask to give you oxygen
· Urinary catheter draining your bladder until you are able to do this or go to the toilet yourself. The catheter is either placed
in the urethra or through your lower abdomen. The catheter can be easily removed in the room.
· Vaginal pack: A cotton gause is rolled up and placed inside the vagina at the end of the operation to help prevent bleeding
and is removed the following morning.
· Naso-gastric tube: passing through your nostril to your stomach
How long does the operation take?
The operation only takes about Twenty-Fourty minutes.. However if Hysterectomy or Prolapse surgery are added the surgery is longer.
Pain
Pain is controlled by either injections, patient controlled anaesthesia, rectal pessaries or tablets. To keep you pain free, you will have injection every four to six hours. Alternatively you may have patient-control anaesthesia (PCA).You press a hand-held device to relieve your pain when you are in discomfort and require pain relief. If you are using PCA, an oxygen mask or nasal canula help you to maintain your normal oxygen level while the infusion is still in progress.
Catheter
If you have had prolapse surgery at the same time, a suprapubic catheter may be left in the bladder.
The suprapubic catheter will be clamped the next day and you will be encouraged to pass urine. After passing urine the suprapubic catheter will then be released to assess the amount left behind. If urine left behind is less than 150 mls the nurses will remove the catheter.
You may not have a catheter and you will be encouraged to pass urine. You may be able to pass urine few hours after surgery. An ultrasound scan will be performed to check that you are able to empty your bladder satisfactorily.
Complications of Tension Free Vaginal Tape are rare and include:
· Bleeding
· Infection
· Bladder Trauma [one per cent]. The surgeon will perform a cystoscopy to be sure that the bladder is not injured.
· Difficulty in emptying bladder [five per cent]
· Go home with a catheter and readmitted to hospital for a trial of void without catheter
· You may have to learn how to self catheterisation [very rare]. Temporarily self catheterization is taught to allow recovery of
the bladder and urethra and onset of spontaneous urination.
· You may experience urge to pass urine [five per cent]
· Pre-existing urgency or urge incontinence may get worse
· You may develop de novo [new] urge incontinence following TVT
· Urinary tract infections occur in five per cent of women after the procedure. Urinary tract and is treated with antibiotics.
· If difficulty in passing urine or severe urgency persists and does not respond to drug therapy, the tape may have to be
divided
· If you continue to experience stress incontinence after surgery further urodynamic studies will be performed to assess if you
require further surgery.
Who will perform the surgery?
Mr Serag Youssif will perform your surgery. An assistant is also present at surgery.
Full information about surgery is discussed with you well prior to surgery.
When can I eat and drink after surgery?
You can eat and drink when you are awake enough. The nurse in charge of your care will decide when and what you can eat or drink. Occasionally you feel sick following surgery and food is held for a little longer.
Going Home
You will be able to go home after you pass urine. If you have had additional surgery such as hysterectomy or vaginal repair you will need to stay in for 3-5 days.
Can I go home in public transport?
No you should arrange for an adult to take you home in a private car or taxi.
Normal Activities
You may be able to resume most normal activities within 1 to 2 weeks.
Driving
You are strongly advised to contact your insurance company to check when you can drive a motor car after your surgery. You can drive when you are able to break suddenly without pain. Generally it takes you 2 weeks to do so without pain.
Intercourse
You are advised to refrain from sexual intercourse for 6 weeks to allow healing.
Heavy Lifting
You should avoid heavy lifting or strenuous activities for 3 months.
After Leaving the Hospital
If you have any problem you should contact
St George Clinic for Women on 9848 4262 OR
Mr Serag Youssif on 0412 062 207 OR
The Hospital you had your surgery at. The nursing staff is always happy to discuss any concern or answer your question.

 |
Tension Free Vaginal Tape Needles Introducer Serag Youssif |
|
 |
Tension Free Vaginal Tape and Needles Serag Youssif |
|
 |
Tension Free Vaginal Tape Needles and Introducer Serag Youssif |
|
 |
Tension Free Vaginal Tape Needles In-Situ Serag Youssif |
|
 |
Tension Free Vaginal Tape Needles In-Situ Serag Youssif |
|
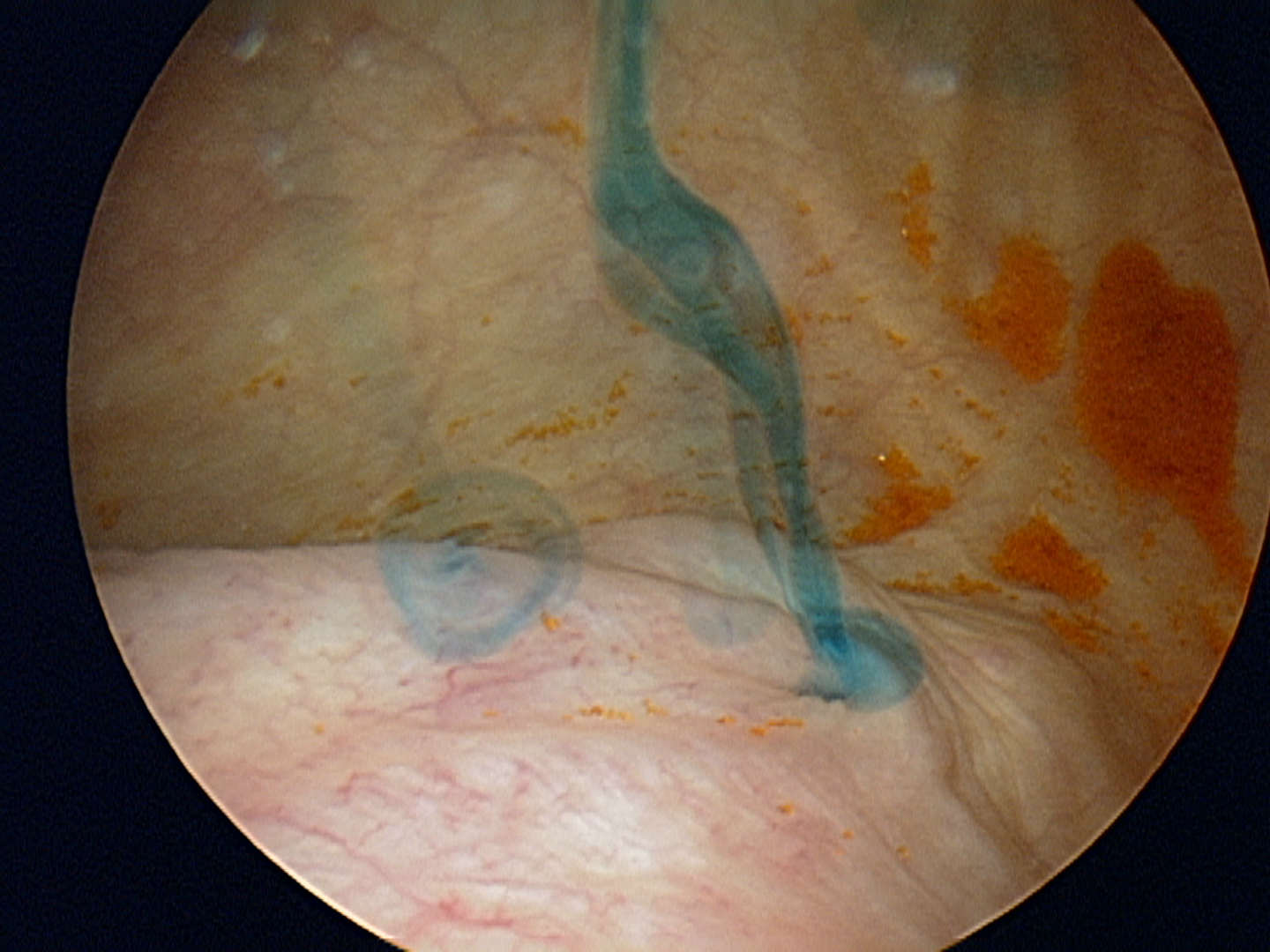 |
indigo carmine jet left ureter |
|
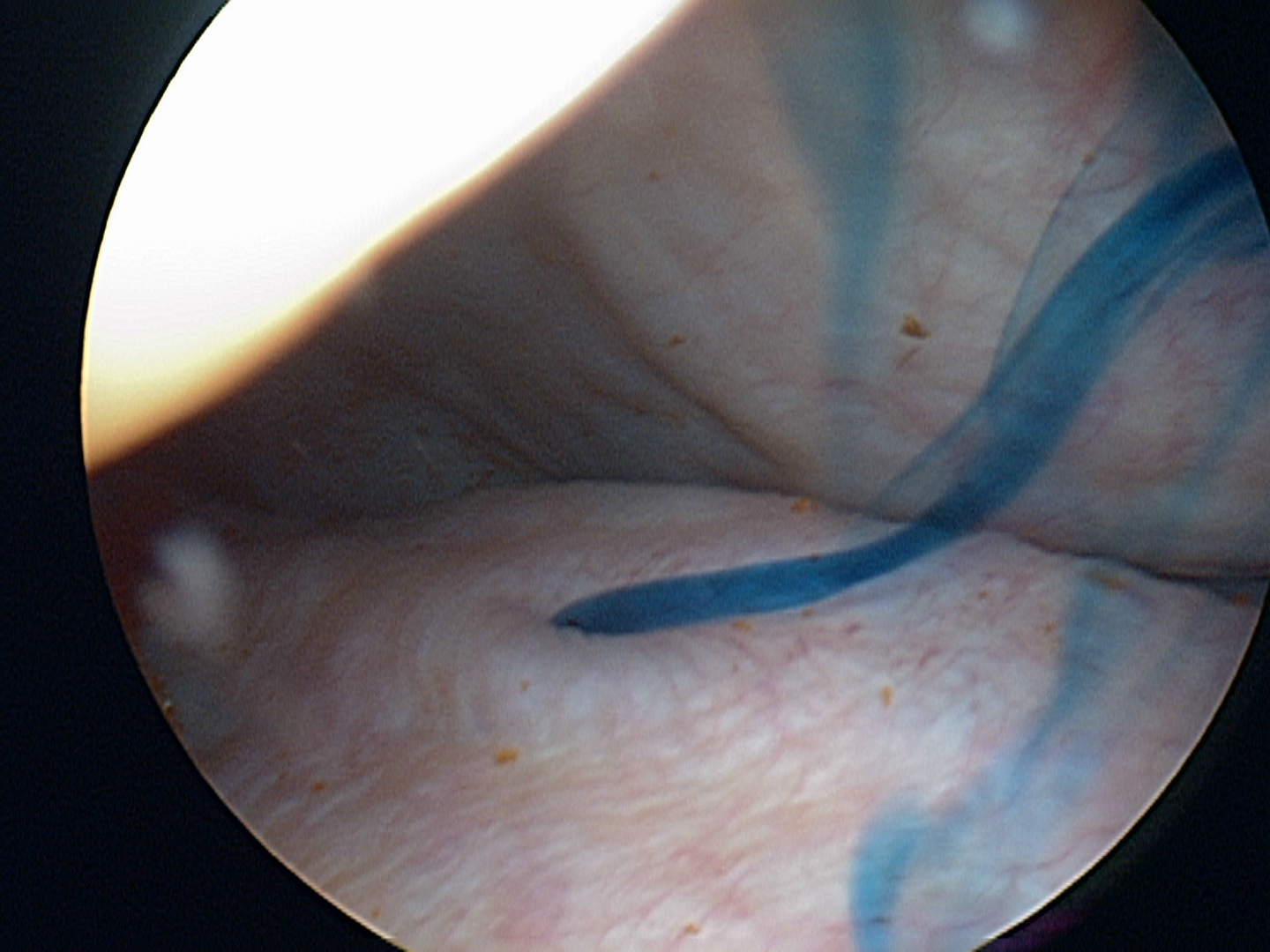 |
indigo jet right ureter serag youssif |
|
